What You Should Know: - Availity today announced a definitive agreement to acquire the utilization management solution and business unit from healthcare automation company Olive AI, Inc. Financial details of the acquisition were not disclosed. - The acquisition of Olive AI's utilization management solution offers numerous benefits for Availity’s national network of payers and providers. These include lower administrative and medical costs, improved patient access
Read More
Utilization Management
Halifax Health Partners with XSOLIS for Precision Hospital Utilization Reviews
What You Should Know: - Today, XSOLIS, the AI technology company creating a more efficient healthcare system, announced a new partnership with Florida-based Halifax Health to achieve greater efficiencies between its utilization management and physician advisor teams across its three hospitals. - XSOLIS’ CORTEX® platform will help Halifax solve administrative challenges and mitigate revenue risk associated with misaligned care level status. CORTEX’s advanced case management analytics
Read More
It’s Time to Stop Accepting the Payer-Provider Dynamic as ‘Adversarial’ and Work Toward Alignment
Today’s relationship between payers and providers is more fraught than ever. With a history of transactional, often adversarial, fee-for-service contract negotiations, it’s no wonder that the healthcare industry has grown too comfortable pitting payers and providers against each other. The lack of trust and transparency between the two groups has led to a perceived misalignment of vision. Across the board, the administrative staff has shouldered the brunt of this friction, which in the end
Read More
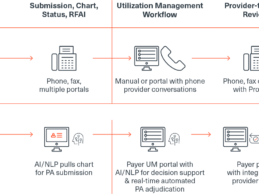
Why It’s Time for Intelligent Prior Authorization
The Centers for Medicare & Medicaid Services (CMS) recently proposed a new rule to advance interoperability and improve the prior authorization (PA) process for Medicare and Medicaid patients. Specifically, the rule stipulates that health plans adopt electronic prior authorization processes, adhere to shorter turnaround times, clearly communicate denial reasons, publish key metrics annually, and implement the Fast Healthcare Interoperability Resources (FHIR) Application Programming Interface
Read More
Edifecs and VirtualHealth Partner to Automate Prior Authorization
What You Should Know: - Today, Edifecs and VirtualHealth, a medical management company, announced a new partnership automated prior authorization to VirtualHealth’s HELIOS® platform for healthcare payer and provider clients. - The Edifecs solution will automate and optimize the prior authorization process across HELIOS to significantly reduce the administrative burden, alleviate friction between payers and providers, and ultimately expedite patient care. Growing Need for Automated Prior
Read More
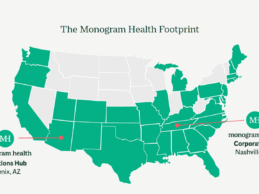
Monogram Health Secures $375M to Expand In-Home Kidney Care
What You Should Know: - Monogram Health, a Nashville, TN-based kidney disease benefit management and care delivery company announced a $375M growth funding round that will drive the company’s continued rapid expansion as the leading solution for high-quality, in-home care for polychronic patients living with chronic kidney and end-stage renal disease in the U.S. - Investors in the round include CVS Health, Cigna, Humana, Memorial Hermann Health System, SCAN, TPG Capital, Frist Cressey
Read More
Edifecs Partners with Empowered-Home to Deliver Automated Prior Authorizations
What You Should Know: - Edifecs and Empowered-Home announced a partnership to provide automated prior authorizations to medical associations, Accountable Care Organizations (ACOs), Independent Physician Associations (IPAs), medical groups, and home health care agencies. - The Edifecs prior authorization solution combined with the clinical decision support system of patient management software company, Privis Health, forms the backbone of Empowered-Home’s ecosystem. Empowered-Home is
Read More
Edifecs Launches Solution to Automate Prior Authorization at the Point of Care
What You Should Know: - The full automation of prior authorization at the point of care leads to improved member experiences, enhanced outcomes, ongoing compliance, and reduced administrative burden. Edifecs’ automated prior authorization solution integrates with electronic health records (EHR) and leverages artificial intelligence (AI), natural language processing (NLP), and industry standards such as FHIR to instantly deliver authorization. - This innovation comes on the heels of
Read More
HealthTeam Advantage Integrates With Bamboo Health’s Pings Solution
What You Should Know: - Bamboo Health™ recently announced that HealthTeam Advantage (HTA), the business name of Care N’ Care Insurance Company of North Carolina, Inc., has integrated Bamboo Health’s Pings™ solution. - The Pings rollout delivers real-time admission, discharge, and transfer (ADT) e-notifications for HTA’s 15,000 North Carolina PPO and HMO Medicare Advantage plan members. Using Real-Time E-Notifications to Lower Costs and Improving High Quality Care Bamboo Health
Read More
Apixio Launches Real-Time Health Data Management Solution
What You Should Know: - Apixio, today, announced the launch of Apicare ChartSpace™, a health data management solution that provides real-time data access to centralized medical charts, accelerated chart and audit file retrieval, and enables the surfacing of actionable insights across value-based care programs. - Apicare ChartSpace centralizes health data, improves security and efficiency of data sharing across departments and external partners, and powers Apixio’s AI-Driven
Read More